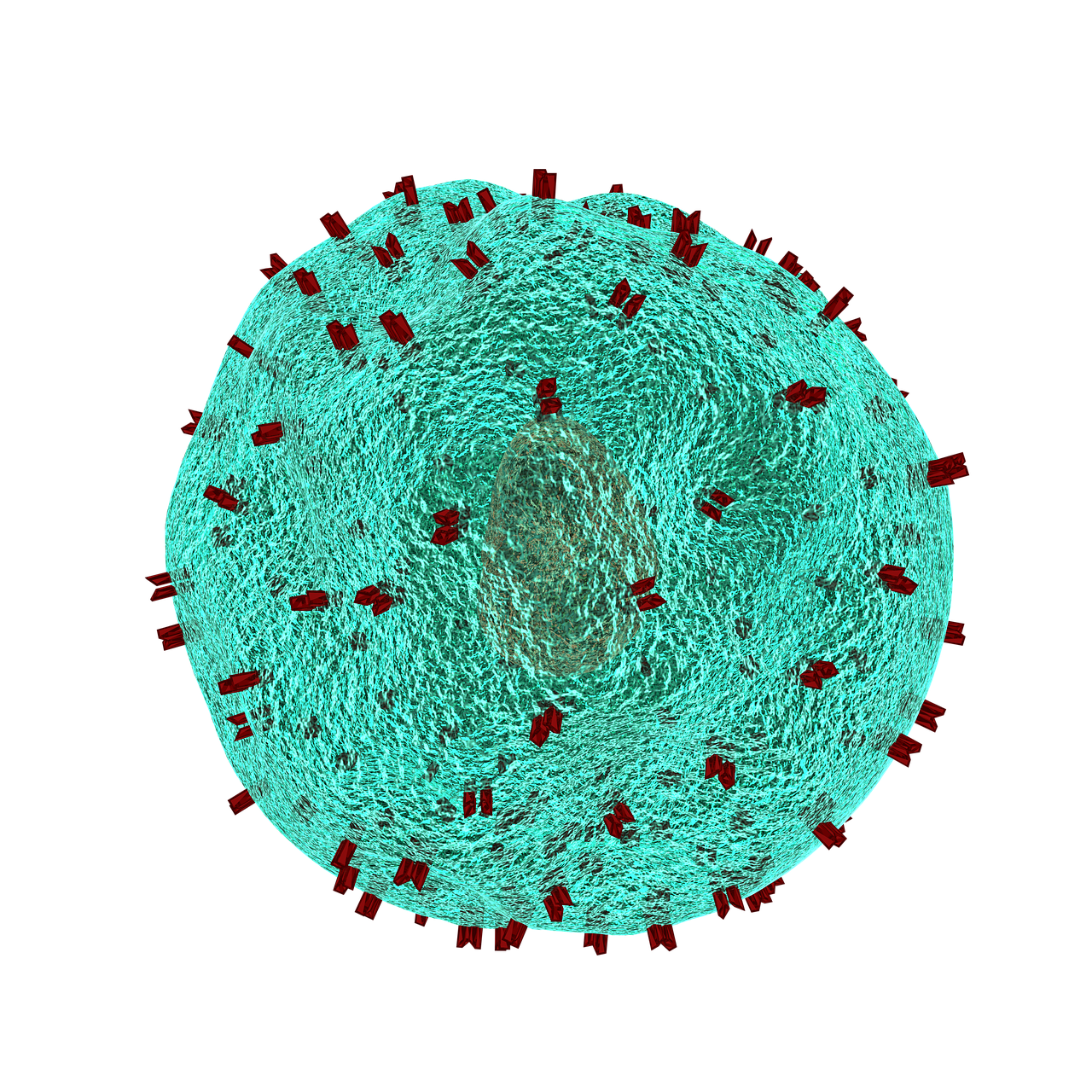
CAR T-cell therapy has transformed treatment for some blood cancers and is being tested in solid tumors, where dense tumor microenvironments, limited T-cell penetration and antigen heterogeneity pose major challenges.
Research presented at the 2025 ASCO Annual Meeting identified claudin 18.2 (CLDN18.2) as a therapeutic target in gastric and gastroesophageal junction cancer (G/GEJC) and reported results for satricabtagene autoleucel (satri-cel; CT041), an autologous CAR T-cell therapy targeting CLDN18.2.
A phase II, open-label, multicenter randomized trial (NCT04581473) enrolled 156 patients in China with advanced CLDN18.2-positive G/GEJC who had progressed after at least two prior systemic therapies. Patients were assigned 2:1 to receive satri-cel (up to three infusions of 250 million cells) or treatment of physician’s choice (TPC), which included apatinib, paclitaxel, docetaxel, irinotecan or nivolumab. Crossover to satri-cel was permitted for patients in the TPC arm after progression or toxicity.
This was a high-risk population: median prior therapies was two, many had three or more, most had peritoneal metastases and Lauren diffuse or mixed histology. Median follow-up was 8.90 months for progression-free survival (PFS) and 12.29 months for overall survival (OS).
In the intention-to-treat population, median PFS was 3.25 months with satri-cel versus 1.77 months with TPC (hazard ratio [HR] 0.366; 95% CI, 0.241–0.557; P < .0001). Median OS was 7.92 months versus 5.49 months (HR 0.693; 95% CI, 0.457–1.051; one-sided P = .0416). Among patients who received the assigned therapy, median PFS was 4.37 months with satri-cel versus 1.84 months with TPC (HR 0.304; 95% CI, 0.195–0.474) and median OS was 8.61 months versus 5.49 months (HR 0.601; 95% CI, 0.385–0.939). Patients who crossed over from TPC to satri-cel had a median OS of 9.20 months.
The safety profile was consistent with CAR T-cell therapies. Treatment-related adverse events (TRAEs) occurred in nearly all satri-cel recipients. Cytokine release syndrome (CRS) occurred in 95.5% of patients, predominantly grade 1–2; 4.5% experienced grade 3 CRS. No immune effector cell-associated neurotoxicity syndrome (ICANS) cases were reported. Serious treatment-related adverse events occurred in 35.2% of patients and treatment-related deaths were rare. Patients in the TPC arm had fewer TRAEs and no CRS.
Oncology nursing implications include vigilance for fever, hypotension and hypoxia as early signs of CRS and prompt management with antipyretics, fluids and other indicated therapies. Nurses are central to patient and caregiver education before leukapheresis, during CAR T-cell manufacturing and lymphodepletion, and after infusion, including monitoring for hematologic toxicities, infections and other complications. Coordination across specialized centers and clear communication about expectations at each step can improve safety and patient experience.
Satri-cel demonstrated meaningful clinical activity in heavily pretreated CLDN18.2-positive G/GEJC with a manageable safety profile and represents a promising CAR T-cell approach in solid tumors. Clinical teams should be prepared for high rates of CRS and the logistical demands of CAR T-cell therapy.
Qi C, Liu C, Peng Z, et al. Claudin-18.2-specific CAR T cells (satri-cel) versus treatment of physician’s choice for previously treated advanced gastric or gastroesophageal junction cancer: primary results from a randomized, open-label, phase II trial (CT041-ST-01). J Clin Oncol. 2025;43(16_suppl):4003. doi:10.1200/JCO.2025.43.16_suppl.4003
Leave a Reply